Lameness is a pain-avoidance strategy adopted by
horses, and is a common cause of poor athletic performance and
compromised welfare. Whatever the precise cause of pain (e.g.
osteoarthritis, tendon injury), that pain is caused by
inflammation.
Inflammation is the cascade of chemical and cellular events that
occurs following any type of tissue damage. By causing pain it alerts the
animal to rest the damaged area, thereby preventing further injury. Inflammation
also acts as the initial stimulant of the healing or repair process, hence it
is extremely important. However ongoing, uncontrolled inflammation causes
chronic pain and can actually exacerbate the tissue damage. This is where
veterinary intervention becomes necessary.
Conventional therapies aim to stop the inflammatory process, and
these remain a vital, cost-effective component of orthopaedic disease
treatment. However, they do not influence the repair of tissue and can
occasionally delay this important process.
‘Regenerative therapies’ aim to optimise the repair of a structure
by replacing damaged tissue with tissue of the same cell type and hope to
minimise the formation of non-functional scar tissue, hence maintaining the
original biomechanical properties of the structure. This increases the
probability of return to previous athletic
ability, and reduces the likelihood of ongoing lameness and/or reinjury.
Research and clinical trials of regenerative therapies have been
ongoing since 2003, but there are now several exciting options that have been
scientifically proven to modify inflammation and reduce pain in clinical
trials, all of which are available at Oakhill.
Stem cells are
a type of cell which have the potential to develop into a variety of more
specialist cell types dependant on the environmental signalling that they are
subject to. An embryo begins as a ball of stem cells that go on to develop into
every type of cell required to make a mature being! Stem cells continue to be
present within the body after birth in reduced quantities.
It is not fully understood how stem cells behave when they are
used as a medical treatment – whether they differentiate into the same cell
type as the tissue they are introduced to, or if they modulate the inflammatory
process. Either way, they have been found to decrease or eliminate lameness
when used to treat joint disease, and have the potential to reduce the reinjury
rate when used to treat tendon injuries!
Autologous stem cells are collected from the individual horse that
requires treatment. Bone marrow is collected (most commonly from the sternum)
under sedation and sent away for complex processing to provide a product
containing millions of stem cells.
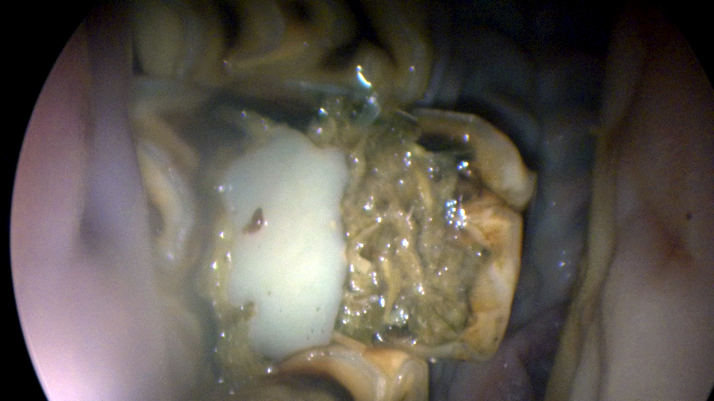
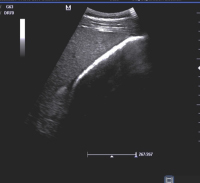
These cells are injected into core (central) lesions within
tendons and ligaments.
Allogenic stem cells are produced from the blood of donor horses
(treated to prevent reaction when introduced into the horse requiring
treatment). These are purified to get rid of other blood cells and then cultured
to increase the number of cells into the millions. They are specifically
stimulated to give the ability to differentiate into chondrocytes – the cell
type present in cartilage.
Commercially this product is available as Arti-Cell. This has
proven highly successful at reducing lameness in horses with degenerative joint
disease.
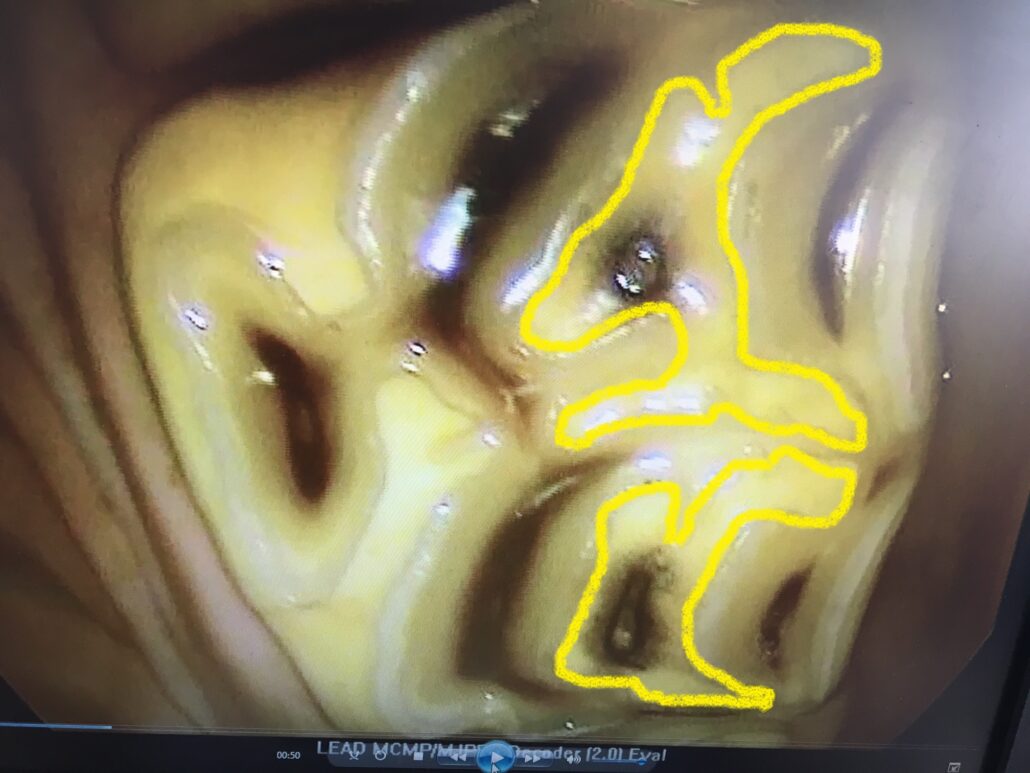
Interleukin-1 Receptor Antagonist Protein, more commonly referred to
as IRAP, is a protein synthesised by a variety of cells. It
prevents the actions of Interleukin-1 – a substance which has an important role
in the induction and maintenance of inflammation within diseased joints.
Studies in humans and horses have proved that intra articular IRAP injections
reduce synovial (joint lining) inflammation and lameness.
IRAP is produced by collection of blood (from the horse to be
treated) in a special syringe. This is then incubated overnight before
filtration to produce concentrated and purified IRAP. This can be frozen to
allow storage of the product until an appropriate time for medication of a
joint. This product can be of benefit where steroid medication is not
appropriate (e.g. competition horses where steroid medication is prohibited,
horses at risk of lamintis) or where joint pain no longer responds to steroid
medication. There is also some evidence that the effects of IRAP last for up to
two years!
Platelet Rich Plasma, or PRP is simply defined as plasma (the none
cellular component of blood) which has been processed to have a high
concentration of platelets. It is rich in growth factors – substances which
stimulate cell multiplication and tissue repair, therefore it promotes a
favourable environment for healing. Like IRAP, it is produced by the specialist
collection and processing of blood (from the horse to be treated). This can be
done immediately prior to injection of the PRP into the area of damage.
PRP is most commonly used in the treatment of ligament injuries
that are not healing as well as anticipated. It is also occasionally used in
the treatment of joint disease that has not responded to steroid medication or
IRAP.
Polyacrylamide hydrogel (marketed for use
in horses as Aquamid) is unlike other regenerative therapies in that it
is a synthetic compound. It is the same material used as a cosmetic filler in
humans! When injected into joints, it becomes integrated into the synovial
membrane (joint capsule) which decreases joint effusion (overproduction of poor
quality joint fluid) and stiffness.
Clinical trials have indicated a high success rate with this
treatment, whether used as a primary treatment or in joints that have failed to
respond to other treatments.
Overall, this is an exciting time for the treatment of equine
lameness. If you wish to discuss the potential benefits of regenerative therapy
for your horse, we would be happy to do so.