Exciting times if your mare is about to foal this season!
A couple of days before parturition the udder of the mare will develop wax tips on the end of the teats.
 A normal birth usually takes about 30 minutes without any help. Directly after the foal is born the umbilicus is still attached. It is important to leave the mare and foal attached for as long as possible. The umbilicus will break at the right time and place, there is no need to cut it. The first couple of hours are important for the foal to drink enough colostrum. Colostrum is full of antibodies necessary for the immunity of the foal.
A normal birth usually takes about 30 minutes without any help. Directly after the foal is born the umbilicus is still attached. It is important to leave the mare and foal attached for as long as possible. The umbilicus will break at the right time and place, there is no need to cut it. The first couple of hours are important for the foal to drink enough colostrum. Colostrum is full of antibodies necessary for the immunity of the foal.
Within 8 hours the foals should drink approximately 2-3 litres of colostrum to get a sufficient enough antibodies.
The foal is only able to take up any antibodies in the first 24hours. If there are any concerns about the uptake of colostrum, a blood sample can be taken to test for IgG levels.
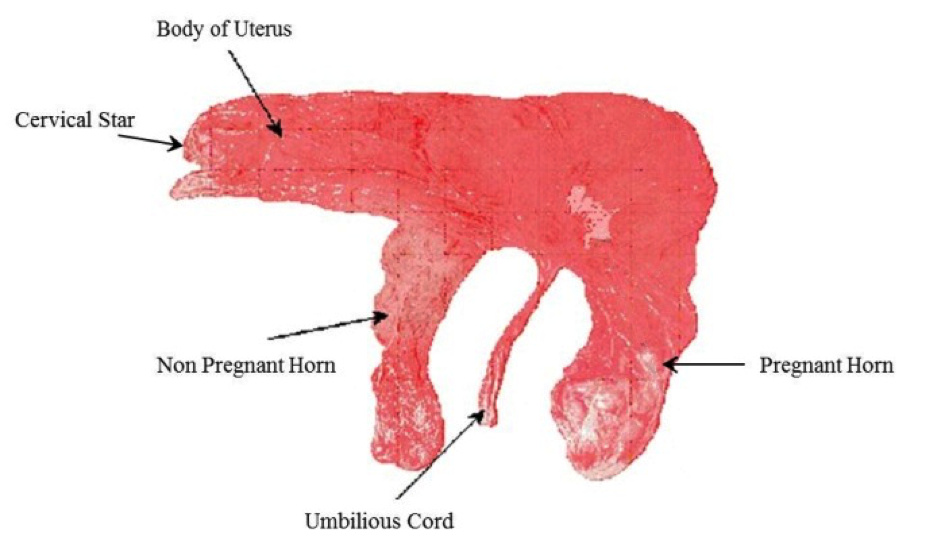 The placenta should be detached from the mare within 4 hours after parturition, it is important to check if the placenta is complete (needs to look like a pair of trousers). If the placenta has not come out within 4 hours, or is not complete it is important to contact the vet.
The placenta should be detached from the mare within 4 hours after parturition, it is important to check if the placenta is complete (needs to look like a pair of trousers). If the placenta has not come out within 4 hours, or is not complete it is important to contact the vet.
Did you know that a healthy foal should:
[checklist icon=”fa-arrow-circle-right” iconcolor=”#39aa87″ circle=”yes”]
-
Lift its head < 5 min
-
Stand < 2 hours
-
Drink < 2 hours
-
Urinate < 6-10 hours
-
Pass yellow feces < 24 hours (after dark meconium)


 Lambing time is the most crucial part of the year for making your sheep business profitable. Lamb deaths from birth to 3 days old should be less than 7% however many farms range between 10- 25%.
Lambing time is the most crucial part of the year for making your sheep business profitable. Lamb deaths from birth to 3 days old should be less than 7% however many farms range between 10- 25%.
 There have been separate cases of Equine Influenza confirmed in the UK. Horses in Essex, Cheshire and Derbyshire have been affected this month with further reports of outbreaks in Belgium, France and Germany. With all three outbreaks it has been unvaccinated horses that have tested positive.
There have been separate cases of Equine Influenza confirmed in the UK. Horses in Essex, Cheshire and Derbyshire have been affected this month with further reports of outbreaks in Belgium, France and Germany. With all three outbreaks it has been unvaccinated horses that have tested positive.
 Horse Flu is endemic in the UK, which means that most horses will come into regular contact with the virus during their lifetime. The control of horse flu in the UK is based on limiting the signs of infection in horses that have been exposed to the virus, rather than trying to prevent exposure itself. This is primarily achieved through regular vaccination which is given either once or twice a year.
Horse Flu is endemic in the UK, which means that most horses will come into regular contact with the virus during their lifetime. The control of horse flu in the UK is based on limiting the signs of infection in horses that have been exposed to the virus, rather than trying to prevent exposure itself. This is primarily achieved through regular vaccination which is given either once or twice a year.